Volume 2, Issue 3 (August 2023)
Health Science Monitor 2023, 2(3): 210-216 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mahmodlou R, Yusefzadeh H, Farjami A, Nabilou B. Cost–effectiveness analysis of jejunostomy tube feeding versus conventional nutritional method in esophageal cancer: a retrospective case control study. Health Science Monitor 2023; 2 (3) :210-216
URL: http://hsm.umsu.ac.ir/article-1-114-en.html
URL: http://hsm.umsu.ac.ir/article-1-114-en.html
Associate Professor. Department of Health Economics and Management, School of Public Health, Social Determinants of Health Research Center, Urmia University of Medical Sciences, Urmia, Iran.
Full-Text [PDF 291 kb]
(1430 Downloads)
| Abstract (HTML) (2371 Views)
JT: Jejunostomy Tube; ALOS: Average Length of Stay; ICU: Intensive Care Unit
Figure 1 shows the decision tree of the two appropriate nutritional methods for patients undergoing esophagectomy. The effectiveness of esophagectomy was calculated with and without the jejunostomy tube and the index of the cost-effectiveness of each choice was finally calculated, taking into account the costs of the two methods. The effectiveness was considered as the decrease in the median time of the start of oral intake.
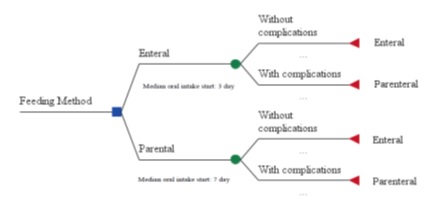
Table 2. ICER of two feeding methods in patients undergoing esophagectomy
ICER: Incremental Cost-Effectiveness Ratio; CNM: Common Nutritional Method; JT: Jejunostomy Tube
Regarding the changing price of vials, solutions, and therefore the hospitalization costs over time, the prices in 2014 were considered as base prices. Thus, one-way sensitivity analysis was used with a 10% decrease in these prices to determine the strength of the results.
With a 10% reduction in prices, the ICER decreased (36 US dollars per day of median duration of oral intake), resulting in a 0.9% reduction in the amount of ICER. So, it can be said that the ratio was not very sensitive to price and showed the strength of the results.
Discussion
This was the first study that aimed to do an economic evaluation of the nutritional approaches in patients undergoing esophagectomy in Iran. The median day of starting oral intake was used as the outcome scale.
As is obvious, the mean consumption of materials (vials and other solutions) and, accordingly, the costs per patient were higher in the control group than in the tube feeding group. This confirms that the CNM in patients undergoing esophagectomy is more expensive, compared with JT feeding.
Regarding the median time of the start of enteral intake, it should be noted that the median time of the start of oral intake was shorter in the case group than in the CNM method, as in the control group. In the case group, the median day of the start of oral intake was 0.42 times the median time of the start of oral intake in the control group.
Studies have also shown improvement in outcomes with the tube feeding method. Most studies, like Mazaki–Ebisawa, Kin–fechin, and Osrinatan observed seven days for the median time of the start of oral intake, which confirms the results of this study (19, 20). Fenton also found similar results (21).
The results of this study showed that the length of stay and total hospitalization costs were significantly lower in the case group. Among the related complications, abdominal distension was only significantly more in this group.
Regarding the costs, only direct medical costs were considered as the measure of costs (hospitalization costs and consumables). It was observed that the cost per patient for routine feeding was about 2.15 times that of the JT method.
In this study, in order to facilitate the decision-making for selecting the low-cost and more effective feeding method, the ICER was calculated. As is apparent, ICER was equal to 1,093,736 IRRs per day of median time reduction in enteral intake in JT, compared to the CNM.According to the results, it can be stated that JT is a cost-effective method for feeding patients undergoing esophagectomy. In addition, the World Health Organization has defined cost effectiveness threshold of interventions being less than three times of the country's GDP per capita (22).
The overall tube-related morbidity is low and it can be recommended in patients at risk of morbidity and nutritional support (23). In patients requiring feeding tubes, evidence was not found about the cost-effectiveness of gastrostomy tubes and JT for preventing aspiration (24). Generally, the JT method was cost-effective in this study. One of the benefits of reducing the median time of enteral intake start is a reduced hospital stay. Therefore, it is an advantage of the JT which increases the cost differences with the CNM.
Finally, it should be stated that the study suffers from several limitations. Studies on calculating DALY as an outcome measure have rarely been performed in Iran. Another problem was the lack of information about the indirect costs to patients. But considering the fast discharge of patients in the JT method and also the pain relief, and faster recovery, indirect costs were lower in the JT method.
The study was not limited to investigating the indications and contraindications of JT feeding. Utilization and reducing costs and hospitalization time were also important, especially in a developing country with limited resources.
It is recommended that more cost-effectiveness and cost-utility studies be performed that consider the indirect costs and the effect of these methods on the patient’s quality of life. With such studies, the cost-effectiveness of these nutritional methods can be decided with more certainty in the future.
Conclusions
JT with a lower median time of the start of enteral intake showed that it is a cost-effective method due to fewer complications and better tolerance of the enteral nutrition method in patients with upper gastrointestinal cancer. Also, it led to decreased hospitalization and costs. As a result, JT provided more comfort for patients with an early return to normal life, compared to the routine nutritional method. On the other hand decrease in the costs and average length of stay in hospitals is an important index of performance and utilization in a developing country.
Acknowledgments
Thanks, to the University Vice Chancellor of Research and Technology, Vice Chancellor of health affairs, and Imam Khomeini Hospital authorities that helped us in conducting the project. We also appreciate the Health Information Technology Department in providing access to patients’ medical records.
Ethical Permissions
The project was approved by the ethics committee of the vice deputy of research and technology in UUMS (IR.UMSU.REC. 1394.55) and data collection permission was obtained.
Conflict of interest
The authors have no conflict of interest in this study.
Funding/support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
The raw data supporting the conclusions of this article are available from the authors upon reasonable request.
Full-Text: (1225 Views)
Introduction
Oesophageal cancer is one of the worst and most fatal cancers, as it is usually not diagnosed until very late stages (1). The most common symptom of the disease is dysphagia. Only surgical resection (esophagectomy) in the very early stages can improve the chances of survival of patients with oesophageal cancer (2, 3).
The surgical complications of esophagectomy include anastomotic leakage, the inability to start oral feeding due to the loss of appetite, and pulmonary infection resulting from the delay in oral intake. All these complications result in a prolonged hospitalization period, subsequent related complications, and mandatory venous nutrition for providing the necessary calories and stabilizing the metabolic state. These impose great costs on the patients and on the health system (4,5).
Jejunostomy provides a safe opening for patients in the case of delayed oral intake. Early intake of food and appropriate calories improves the metabolic state and enable the patients to take oral drugs instead of intravenous medication (6). Given that patients confront malnutrition after esophagectomy, jejunostomy can additionally be effective in preventing weight loss (7). Enteral feeding tubes are vital for people who need them because of nutrition, hydration, and medication every day (8). The common complications of jejunostomy include obstruction, tube displacement, infection of the insertion site on the abdomen, and metabolic problems (9).
Considering the cultural and economic differences between Iran and developed countries, a significant number of patients in Iran are unable to receive adequate food and calories. In addition, some patients do not have a good appetite due to the complications of anesthesia and surgery. Moreover, in cases where the patients have anastomotic leakage, oral intake is unsuitable. Usually, hospitalization of these patients and performing Total Parenteral Nutrition (TPN) are necessary for providing the required calories in such cases (10). Nevertheless, TPN has its own side effects and imposes high costs on the patients and on the healthcare system (11).
On the other hand, enteral feeding has many benefits, such as an improved immune system and reduced infectious complications (10). In such cases, patients can be fed by Jejunostomy Tube (JT), discharged early; and even they wait for anastomosis closure (12). Galhego reported jejunostomy as an efficient and safe method of early nutrition (13).
Studies have shown mixed results in terms of the effectiveness of jejunostomy. In a study conducted by Sadeesh, the results indicated that routinely performing a jejunostomy increases complications (6). However, in another study done between 2003 and 2007 by Vikus Gupta et al., it was demonstrated that this method reduced surgical complications by providing nutritional support, especially in patients with anastomoses leak, and was recommended for routine use after procedures to treat gastric and oesophageal cancers (12).
To the best of our knowledge, no study has been conducted on the economic evaluation of jejunostomy on such patients. The present study aimed to investigate the cost–effectiveness of JT in patients with oesophageal cancer who underwent esophagectomy, compared to those who fed by the Common Nutritional Method (CNM) to determine whether performing JT saves costs and time for hospitals and patients undergoing esophagectomy.
Materials & Methods
Design:
This retrospective case-control study was conducted in a five-year time frame, at the largest referral hospital affiliated with Urmia University of Medical Sciences (UUMS), Iran in 2015. The aim of the study was to analyse the cost–effectiveness of two feeding methods in patients who underwent esophagectomy: 1) the JT method (enteral group), 2) the CNM method.
Cost-Effectiveness analyses:
Inputs included costs of hospitalization, drugs, and solutions. The final outcome of the jejunostomy was considered as a criterion of effectiveness. In this way, the median time to start oral feeding was considered as the unit of effectiveness. To calculate the cost-effectiveness ratio in each of the designated strategies, the total cost of treatment was divided into the median time to start the oral feeding period after the main surgery.
After comparing the hospital costs between patients feeding with JT and those with CNM, and related analyses, the usefulness of JT in studied patients was discussed. The incremental Cost-Effectiveness Ratio (ICER) was used to compare selected strategies. In this way, the costs spent on a strategy with less effectiveness were deducted from the costs spent on the strategy with more effectiveness. Finally, ICER was calculated by dividing the result by the difference in the effectiveness of these two strategies (14, 15).
ICER= (Cost A – Cost B)/ (Outcome A – Outcome B)
A larger ICER means that more money is needed to buy each unit of outcome and intervention is less cost-effective (16). To increase the accuracy of work and due to the inherent uncertainty of data, Sensitivity analysis was used after the calculation of incremental cost-effectiveness. The sensitivity analysis shows how much the results are sensitive to fluctuations and to what extent it is generalizable (17, 18).
Jejunostomy procedure:
All procedures were the same in all patients and were performed with the same surgeon. The jejunostomy tube is embedded by the Stamm method. Esophagectomy and jejunostomy were simultaneously performed in the JT group.
Subjects:
The population of the study included patients with oesophageal cancer who underwent esophagectomy from 2010 to 2014. All 50 patients who underwent laparoscopic feeding jejunostomy following esophagectomy for upper gastrointestinal malignancies were chosen as case group by census method and due to the limited number of patients, sampling was not performed. The control group consisted of 50 patients who had undergone esophagectomy without JT, with the same surgeon, in the same time period, and at the same center.
All patients in the two groups were in stages 2 or 3 of esophageal cancer. Patients received chemotherapy or chemoradiotherapy prior to surgery according to the results of the pathology. All patients had the same socio-economic conditions in two groups.
Data collection and statistical analyses:
The medical records of all patients in the two groups were retrospectively reviewed between January 2010 and December 2014. The required data including esophagectomy and jejunostomy costs, hospitalization days (ward and ICU), solutions costs, and medication costs in both groups were extracted and recorded.
A discount rate of 5 % was applied for calculating costs. After calculating and comparing all costs in both groups and analysing data, the comparative benefits of the two methods were investigated in the study population. The description and the analysis were performed using the SPSS, version 16. The statistical significance level of tests was defined at p<05.
Results
In this study, the mean age of the patients was 64.7 years in the case group and 63.9 years in the control group. In this group, 27(54%) patients were male. The mean of weight loss in the JT group was less than the control group, but the difference was not statistically significant (p> 0.5). Table 1 demonstrates the demographics, clinical characteristics, and cost items comparison between the two groups studied.
Patients were NPO for at least 5 days after the intervention in two groups. NPO lasted more than 5 days in case of anastomosis leakage. Considering that the JT position was distal to the anastomosis, after the resolution of the ileus and the lack of contraindications, intestinal nutrition started through the JT.
Patients in the case group were hospitalized until complete dietary intake. Patients in the JT group were discharged as soon as they tolerated a clear liquid diet and enteral nutrition training. The JT was removed after assuring the regime's tolerance after a week.
In the case group, gavage solutions including carbohydrates, protein, fat, vitamins, and required minerals were used. The consumption of albumin, intralipid, and amino fusion vials in the control group was 15, 7, and 14 per person, respectively.
The cost of the consumed albumin was 65 US dollars, of intralipid was 12.76 US dollars, and of amino fusion vials was 13 US dollars per patient. Therefore, the total costs of taking these vials in the control group were 1213 US dollars per patient. The costs in the case group were zero in this context. The mean cost of gavage solutions per patient in the case group was 38 US dollars.
In this study, the average length of stay was directly associated with the time to start enteral intake. In the case group, the median of enteral intake start was three days and the average length of stay was significantly shorter, compared to the control group with a median of oral intake start at seventh days. The average total hospitalization costs (including the cost of jejunostomy) per patient suffering from oesophageal cancer in the case group and the control group were 2228 and 3666 US dollars, respectively.
Table 1. Demographic and clinical information of patients undergoing esophagectomy in studied groups
Oesophageal cancer is one of the worst and most fatal cancers, as it is usually not diagnosed until very late stages (1). The most common symptom of the disease is dysphagia. Only surgical resection (esophagectomy) in the very early stages can improve the chances of survival of patients with oesophageal cancer (2, 3).
The surgical complications of esophagectomy include anastomotic leakage, the inability to start oral feeding due to the loss of appetite, and pulmonary infection resulting from the delay in oral intake. All these complications result in a prolonged hospitalization period, subsequent related complications, and mandatory venous nutrition for providing the necessary calories and stabilizing the metabolic state. These impose great costs on the patients and on the health system (4,5).
Jejunostomy provides a safe opening for patients in the case of delayed oral intake. Early intake of food and appropriate calories improves the metabolic state and enable the patients to take oral drugs instead of intravenous medication (6). Given that patients confront malnutrition after esophagectomy, jejunostomy can additionally be effective in preventing weight loss (7). Enteral feeding tubes are vital for people who need them because of nutrition, hydration, and medication every day (8). The common complications of jejunostomy include obstruction, tube displacement, infection of the insertion site on the abdomen, and metabolic problems (9).
Considering the cultural and economic differences between Iran and developed countries, a significant number of patients in Iran are unable to receive adequate food and calories. In addition, some patients do not have a good appetite due to the complications of anesthesia and surgery. Moreover, in cases where the patients have anastomotic leakage, oral intake is unsuitable. Usually, hospitalization of these patients and performing Total Parenteral Nutrition (TPN) are necessary for providing the required calories in such cases (10). Nevertheless, TPN has its own side effects and imposes high costs on the patients and on the healthcare system (11).
On the other hand, enteral feeding has many benefits, such as an improved immune system and reduced infectious complications (10). In such cases, patients can be fed by Jejunostomy Tube (JT), discharged early; and even they wait for anastomosis closure (12). Galhego reported jejunostomy as an efficient and safe method of early nutrition (13).
Studies have shown mixed results in terms of the effectiveness of jejunostomy. In a study conducted by Sadeesh, the results indicated that routinely performing a jejunostomy increases complications (6). However, in another study done between 2003 and 2007 by Vikus Gupta et al., it was demonstrated that this method reduced surgical complications by providing nutritional support, especially in patients with anastomoses leak, and was recommended for routine use after procedures to treat gastric and oesophageal cancers (12).
To the best of our knowledge, no study has been conducted on the economic evaluation of jejunostomy on such patients. The present study aimed to investigate the cost–effectiveness of JT in patients with oesophageal cancer who underwent esophagectomy, compared to those who fed by the Common Nutritional Method (CNM) to determine whether performing JT saves costs and time for hospitals and patients undergoing esophagectomy.
Materials & Methods
Design:
This retrospective case-control study was conducted in a five-year time frame, at the largest referral hospital affiliated with Urmia University of Medical Sciences (UUMS), Iran in 2015. The aim of the study was to analyse the cost–effectiveness of two feeding methods in patients who underwent esophagectomy: 1) the JT method (enteral group), 2) the CNM method.
Cost-Effectiveness analyses:
Inputs included costs of hospitalization, drugs, and solutions. The final outcome of the jejunostomy was considered as a criterion of effectiveness. In this way, the median time to start oral feeding was considered as the unit of effectiveness. To calculate the cost-effectiveness ratio in each of the designated strategies, the total cost of treatment was divided into the median time to start the oral feeding period after the main surgery.
After comparing the hospital costs between patients feeding with JT and those with CNM, and related analyses, the usefulness of JT in studied patients was discussed. The incremental Cost-Effectiveness Ratio (ICER) was used to compare selected strategies. In this way, the costs spent on a strategy with less effectiveness were deducted from the costs spent on the strategy with more effectiveness. Finally, ICER was calculated by dividing the result by the difference in the effectiveness of these two strategies (14, 15).
ICER= (Cost A – Cost B)/ (Outcome A – Outcome B)
A larger ICER means that more money is needed to buy each unit of outcome and intervention is less cost-effective (16). To increase the accuracy of work and due to the inherent uncertainty of data, Sensitivity analysis was used after the calculation of incremental cost-effectiveness. The sensitivity analysis shows how much the results are sensitive to fluctuations and to what extent it is generalizable (17, 18).
Jejunostomy procedure:
All procedures were the same in all patients and were performed with the same surgeon. The jejunostomy tube is embedded by the Stamm method. Esophagectomy and jejunostomy were simultaneously performed in the JT group.
Subjects:
The population of the study included patients with oesophageal cancer who underwent esophagectomy from 2010 to 2014. All 50 patients who underwent laparoscopic feeding jejunostomy following esophagectomy for upper gastrointestinal malignancies were chosen as case group by census method and due to the limited number of patients, sampling was not performed. The control group consisted of 50 patients who had undergone esophagectomy without JT, with the same surgeon, in the same time period, and at the same center.
All patients in the two groups were in stages 2 or 3 of esophageal cancer. Patients received chemotherapy or chemoradiotherapy prior to surgery according to the results of the pathology. All patients had the same socio-economic conditions in two groups.
Data collection and statistical analyses:
The medical records of all patients in the two groups were retrospectively reviewed between January 2010 and December 2014. The required data including esophagectomy and jejunostomy costs, hospitalization days (ward and ICU), solutions costs, and medication costs in both groups were extracted and recorded.
A discount rate of 5 % was applied for calculating costs. After calculating and comparing all costs in both groups and analysing data, the comparative benefits of the two methods were investigated in the study population. The description and the analysis were performed using the SPSS, version 16. The statistical significance level of tests was defined at p<05.
Results
In this study, the mean age of the patients was 64.7 years in the case group and 63.9 years in the control group. In this group, 27(54%) patients were male. The mean of weight loss in the JT group was less than the control group, but the difference was not statistically significant (p> 0.5). Table 1 demonstrates the demographics, clinical characteristics, and cost items comparison between the two groups studied.
Patients were NPO for at least 5 days after the intervention in two groups. NPO lasted more than 5 days in case of anastomosis leakage. Considering that the JT position was distal to the anastomosis, after the resolution of the ileus and the lack of contraindications, intestinal nutrition started through the JT.
Patients in the case group were hospitalized until complete dietary intake. Patients in the JT group were discharged as soon as they tolerated a clear liquid diet and enteral nutrition training. The JT was removed after assuring the regime's tolerance after a week.
In the case group, gavage solutions including carbohydrates, protein, fat, vitamins, and required minerals were used. The consumption of albumin, intralipid, and amino fusion vials in the control group was 15, 7, and 14 per person, respectively.
The cost of the consumed albumin was 65 US dollars, of intralipid was 12.76 US dollars, and of amino fusion vials was 13 US dollars per patient. Therefore, the total costs of taking these vials in the control group were 1213 US dollars per patient. The costs in the case group were zero in this context. The mean cost of gavage solutions per patient in the case group was 38 US dollars.
In this study, the average length of stay was directly associated with the time to start enteral intake. In the case group, the median of enteral intake start was three days and the average length of stay was significantly shorter, compared to the control group with a median of oral intake start at seventh days. The average total hospitalization costs (including the cost of jejunostomy) per patient suffering from oesophageal cancer in the case group and the control group were 2228 and 3666 US dollars, respectively.
| Without JT | Without JT | p value | |
| Age (year) | 63.9 | 63.9 | -- |
| Male | 24(48%) | 24(48%) | -- |
| Female | 26(52%) | 26(52%) | -- |
| ALOS (Total) (days) | 12.8 | 12.8 | 0.02 |
| ALOS (ICU) (days) | 5.2 | 5.2 | 0.09 |
| Median oral intake start (days) | 7 | 7 | 0.002 |
Pneumonia (Number) |
3 | 3 | 0.91 |
| Abdominal distension (Number) | 2 | 2 | 0.04 |
| Anastomotic leak (Number) | 4 | 4 | 0.88 |
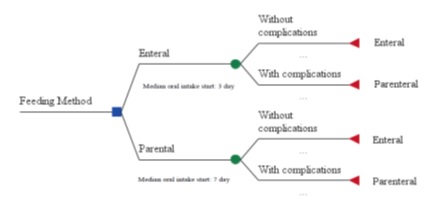
Fig. 1. Decision tree to choose the most appropriate nutritional method in patients undergoing esophagectomy
In this study, the ICER was calculated using the data of costs and outcomes as represented in Table 2. The costs per day of hospitalization of patients in the intervention group were 6109009 IRRs and in the control group were 381 US dollars.
The cost differences of hospitalization of both
methods per patient per day were considered in the numerator and the differences in the median time of oral intake per patient were considered in the denominator. The ICER of JT feeding against CNM was about a 40 US dollars decrease per day in the median time of the start of oral intake.
The cost differences of hospitalization of both
methods per patient per day were considered in the numerator and the differences in the median time of oral intake per patient were considered in the denominator. The ICER of JT feeding against CNM was about a 40 US dollars decrease per day in the median time of the start of oral intake.
Table 2. ICER of two feeding methods in patients undergoing esophagectomy
| Strategy | Cost (US dollars) | Effectiveness | Cost/Effectiveness | ICER |
| CNM | 381 | 7 | 54 | - |
| JT | 222 | 3 | 74 | 40 |
With a 10% reduction in prices, the ICER decreased (36 US dollars per day of median duration of oral intake), resulting in a 0.9% reduction in the amount of ICER. So, it can be said that the ratio was not very sensitive to price and showed the strength of the results.
Discussion
This was the first study that aimed to do an economic evaluation of the nutritional approaches in patients undergoing esophagectomy in Iran. The median day of starting oral intake was used as the outcome scale.
As is obvious, the mean consumption of materials (vials and other solutions) and, accordingly, the costs per patient were higher in the control group than in the tube feeding group. This confirms that the CNM in patients undergoing esophagectomy is more expensive, compared with JT feeding.
Regarding the median time of the start of enteral intake, it should be noted that the median time of the start of oral intake was shorter in the case group than in the CNM method, as in the control group. In the case group, the median day of the start of oral intake was 0.42 times the median time of the start of oral intake in the control group.
Studies have also shown improvement in outcomes with the tube feeding method. Most studies, like Mazaki–Ebisawa, Kin–fechin, and Osrinatan observed seven days for the median time of the start of oral intake, which confirms the results of this study (19, 20). Fenton also found similar results (21).
The results of this study showed that the length of stay and total hospitalization costs were significantly lower in the case group. Among the related complications, abdominal distension was only significantly more in this group.
Regarding the costs, only direct medical costs were considered as the measure of costs (hospitalization costs and consumables). It was observed that the cost per patient for routine feeding was about 2.15 times that of the JT method.
In this study, in order to facilitate the decision-making for selecting the low-cost and more effective feeding method, the ICER was calculated. As is apparent, ICER was equal to 1,093,736 IRRs per day of median time reduction in enteral intake in JT, compared to the CNM.According to the results, it can be stated that JT is a cost-effective method for feeding patients undergoing esophagectomy. In addition, the World Health Organization has defined cost effectiveness threshold of interventions being less than three times of the country's GDP per capita (22).
The overall tube-related morbidity is low and it can be recommended in patients at risk of morbidity and nutritional support (23). In patients requiring feeding tubes, evidence was not found about the cost-effectiveness of gastrostomy tubes and JT for preventing aspiration (24). Generally, the JT method was cost-effective in this study. One of the benefits of reducing the median time of enteral intake start is a reduced hospital stay. Therefore, it is an advantage of the JT which increases the cost differences with the CNM.
Finally, it should be stated that the study suffers from several limitations. Studies on calculating DALY as an outcome measure have rarely been performed in Iran. Another problem was the lack of information about the indirect costs to patients. But considering the fast discharge of patients in the JT method and also the pain relief, and faster recovery, indirect costs were lower in the JT method.
The study was not limited to investigating the indications and contraindications of JT feeding. Utilization and reducing costs and hospitalization time were also important, especially in a developing country with limited resources.
It is recommended that more cost-effectiveness and cost-utility studies be performed that consider the indirect costs and the effect of these methods on the patient’s quality of life. With such studies, the cost-effectiveness of these nutritional methods can be decided with more certainty in the future.
Conclusions
JT with a lower median time of the start of enteral intake showed that it is a cost-effective method due to fewer complications and better tolerance of the enteral nutrition method in patients with upper gastrointestinal cancer. Also, it led to decreased hospitalization and costs. As a result, JT provided more comfort for patients with an early return to normal life, compared to the routine nutritional method. On the other hand decrease in the costs and average length of stay in hospitals is an important index of performance and utilization in a developing country.
Acknowledgments
Thanks, to the University Vice Chancellor of Research and Technology, Vice Chancellor of health affairs, and Imam Khomeini Hospital authorities that helped us in conducting the project. We also appreciate the Health Information Technology Department in providing access to patients’ medical records.
Ethical Permissions
The project was approved by the ethics committee of the vice deputy of research and technology in UUMS (IR.UMSU.REC. 1394.55) and data collection permission was obtained.
Conflict of interest
The authors have no conflict of interest in this study.
Funding/support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
The raw data supporting the conclusions of this article are available from the authors upon reasonable request.
Type of Study: Research Article |
Subject:
Health Policy, Management, and Economics
Received: 2023/04/19 | Accepted: 2023/05/22 | Published: 2023/07/19
Received: 2023/04/19 | Accepted: 2023/05/22 | Published: 2023/07/19
References
1. Zhang Y. Epidemiology of esophageal cancer. World journal of gastroenterology: WJG. 2013;19(34):5598. [DOI] [PMID] [PMCID]
2. DeMeester TR, editor Esophageal carcinoma: current controversies. Seminars in surgical oncology; 1997: Wiley Online Library.
https://doi.org/10.1002/(SICI)1098-2388(199707/08)13:4<217::AID-SSU2>3.0.CO;2-8 [DOI]
3. Russell MC, Thourani VH, Miller Jr JI. Modified nissen fundoplication combined with Ivor Lewis esophagogastrectomy. The Annals of thoracic surgery. 2007;84(5):1780-2. [DOI] [PMID]
4. Velanovich V, Mohlberg N. The split-stomach fundoplication after esophagogastrectomy. Journal of gastrointestinal surgery. 2006;10(2):178-85. [DOI] [PMID]
5. Junemann-Ramirez M, Awan M, Khan Z, Rahamim J. Anastomotic leakage post-esophagogastrectomy for esophageal carcinoma: retrospective analysis of predictive factors, management and influence on longterm survival in a high volume centre. European journal of cardio-thoracic surgery. 2005;27(1):3-7. [DOI] [PMID]
6. Srinathan SK, Hamin T, Walter S, Tan AL, Unruh HW, Guyatt G. Jejunostomy tube feeding in patients undergoing esophagectomy. Canadian Journal of Surgery. 2013;56(6):409. [DOI] [PMID] [PMCID]
7. Fanning M, Mc Hugh A, Browne C, Ravi N, Reynolds J, Healy L. PTU-200 Home jejunostomy feeding post-oesophagectomy: a change in practice. Gut. 2012;61(Suppl 2):A267-A. [DOI]
8. Fisher C, Blalock B. Clogged feeding tubes: a clinician's thorn. Pract Gastroenterol. 2014;17. [URL]
9. Júnior LGT, de Vasconcellos Santos FA, Correia MITD. Randomized clinical trial: nasoenteric tube or jejunostomy as a route for nutrition after major upper gastrointestinal operations. World journal of surgery. 2014;38(9):2241-6. [DOI] [PMID]
10. Brunicardi F, Andersen D, Billiar T, Dunn D, Hunter J, Matthews J, et al. Schwartz's principles of surgery, 10e: McGraw-hill; 2014. [Google Scholar]
11. Al Batani R, Abdullah DC, Bahari MB. Evaluation of the total parenteral nutrition service at Universiti Sains Malaysia Hospital. e-SPEN, the European e-Journal of Clinical Nutrition and Metabolism. 2007;2(6):e111-e5. [DOI]
12. Gupta V. Benefits versus risks: a prospective audit. World journal of surgery. 2009;33(7):1432-8. [DOI] [PMID]
13. Galhego R, Moura R, Enne M. Jejunostomy or nasoenteric tube: Which is the best route for nutrition after Whipple procedure. HPB. 2016;18:e370. [DOI]
14. Elliott R, Payne K. Essentials of economic evaluation in healthcare: pharmaceutical press; 2005. [Google Books]
15. Robinson R. Economic evaluation and health care. What does it mean? Bmj. 1993;307(6905):670-3. [DOI] [PMID] [PMCID]
16. Fox-Rushby J, Cairns J. Economic evaluation: McGraw-Hill Education (UK); 2005.17. Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes: Oxford university press; 2015. [URL]
17. Briggs A, Sculpher M, Buxton M. Uncertainty in the economic evaluation of health care technologies: the role of sensitivity analysis. Health economics. 1994;3(2):95-104. [DOI] [PMID]
18. Chin K-F, Townsend S, Wong W, Miller GV. A prospective cohort study of feeding needle catheter jejunostomy in an upper gastrointestinal surgical unit. Clinical Nutrition. 2004;23(4):691-6. [DOI] [PMID]
19. Mazaki T, Ebisawa K. Enteral versus parenteral nutrition after gastrointestinal surgery: a systematic review and meta-analysis of randomized controlled trials in the English literature. Journal of Gastrointestinal Surgery. 2008;12(4):739-55. [DOI] [PMID]
20. Fenton JR, Bergeron EJ, Coello M, Welsh RJ, Chmielewski GW. Feeding jejunostomy tubes placed during esophagectomy: are they necessary? The Annals of thoracic surgery. 2011;92(2):504-12. [DOI] [PMID]
21. Muennig P, Bounthavong M. Cost-effectiveness analysis in health: a practical approach: John Wiley & Sons; 2016. [Google Books]
22. Minarich MJ, Schwarz RE. Experience with a simplified feeding jejunostomy technique for enteral nutrition following major visceral operations. Translational gastroenterology and hepatology. 2018;3. [DOI] [PMID] [PMCID]
23. Brett K, Argáez C. Gastrostomy versus Gastrojejunostomy and/or Jejunostomy Feeding Tubes: A Review of Clinical Effectiveness, Cost-Effectiveness and Guidelines. 2018. [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







 gmail.com
gmail.com